
The claim process is as follows.
1)(Optional, but Recommended) Doctor enters in the EMR Billing screen the items to be billed by selecting the inventory items for each procedure to be billed. The provider saves his billing information (service, CPT and ICD codes) by selecting the check mark button on the tool bar above the EMR billing grid.
2)The invoice/billing staff creates or opens an invoice for the patient. If they create the invoice after the EMR is completed they will be prompted to add the billing items from the EMR. If they have already created the invoice they can select the EMR items by choosing the EMR Unbilled Items button in the invoice. In either situation they can transfer or enter manually into the invoice the EMR billing items.
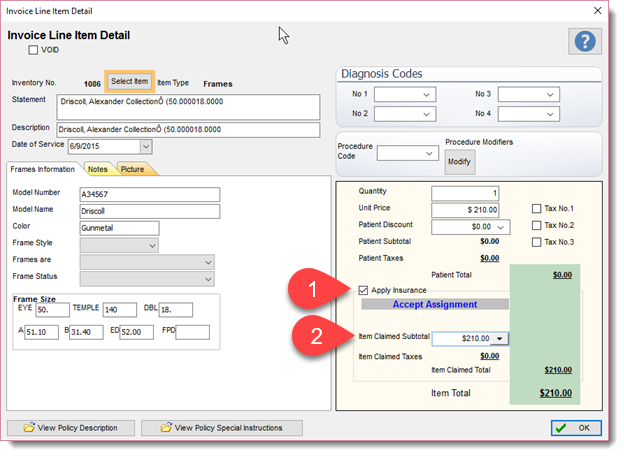
3)Once the items are in the invoice the user can identify which are to be used for claim purposes. Edit each invoice line item (open the Invoice Line Item Detail screen) and mark them (if applicable) to be billed to the insurance. You must have a valid Procedure and Diagnostic code entered. To mark an invoice item for billing to an insurance company place a check mark in the Apply Insurance check box (1). (make any adjustment to the fee if applicable by changing the Item Claimed Subtotal (2) field).
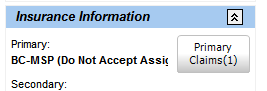
4)Once all items are properly assigned the user then creates the claim by selecting the invoice Insurance button – Primary Claims
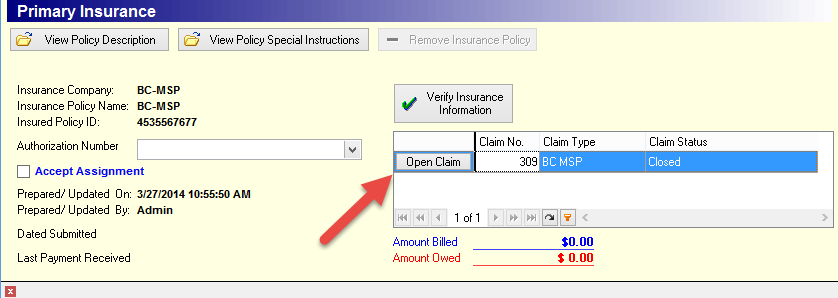
5) Edit the claim by selecting the Open Claim option and complete or edit the claim if required.
6)To send the claim use the Send Claims to Insurance Companies button located in the Back Office – Patient & Insurance tab.
