Warning: Incomplete or erroneous information entered will result in all insurance claim for the invoice to be incorrectly created and rejected by insurance companies. |
To process a claim, the patient must be assigned and have configured an Insurance Company Policy in his patient file. A properly configured Insurance Company and policy profile must exist in the Insurance Manager prior to the invoice being created.
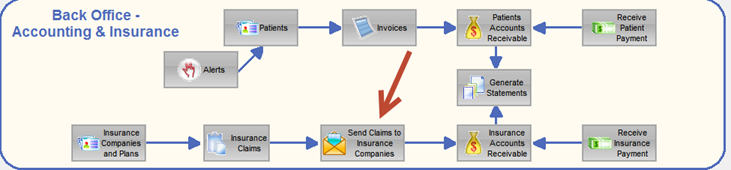
The Invoice is the centralized point where all of the information from the exam, patient, insurance company, provider profile and insurance policy is read and used to prepare a valid insurance claim. The key information needed is entered at invoice time and the claim can be prepared at the same time by the end user. Once the claims is prepared it can be batched for sending to the claim processor.
The upper right portion of the invoice screen contains the office insurance section .
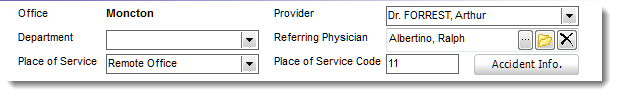
This section contains the billing information needed to identify the office that is creating an insurance claim. If information is missing or incorrect in these fields the insurance claim will be rejected.
Office: The office (branch office) who will be sending the insurance claim. This is equal to the CMS-1500 field 32 . The insurance claim will use this information for billing purposes. It will use the Information you entered in the System Setting section for Offices Settings. It will use the address of the office.
Department: (optional) This field is for internal reporting of sales only and is not used for claim processing. If it is entered, sales report for the various departments can be generated.
Place of Service and code: This is equal to the CMS-1500 field 24b which identifies the place of service to be used for insurance billing purposes. It will enter the Place of Service code you entered in the System Setting section for Place of Service Location and display the CMS-1500 code that will be used for claim purposes.
Provider: This is the Provider making the insurance claim request. Typically it is the Provider that completed the services being billed to the insurance company. The information entered in the Employee - Provider section of the employee file are used for completion of the insurance claim. At creation time, you can change the default provider to another provider. Once the Invoice has been created and saved, this change feature is deactivated.
Referring Physician: The user can select and identify for claims purposes the referring doctor (example: CMS-1500 field 17). You must have a referring physician for the CMS-1500 fields 17, 17a and 17b to be completed. A missing referring physician deactivates these fields. The referring doctor drop down is populated via the Family Physician and referring Doctor database which can be updated via a patient file or the Rolodex. The Referring Doctor NPI number (CMS-1500 17b) is read from the Family Physician and referring Doctor table.
The Accident button relates to the CMS-1500 item 10 "Is Patient's Condition Related To:"
Place a check mark to indicate whether employment, auto accident, or other accident involvement applies to one or more of the services described in the Claim form such as CMS-1500 item 24. Enter the State postal code.
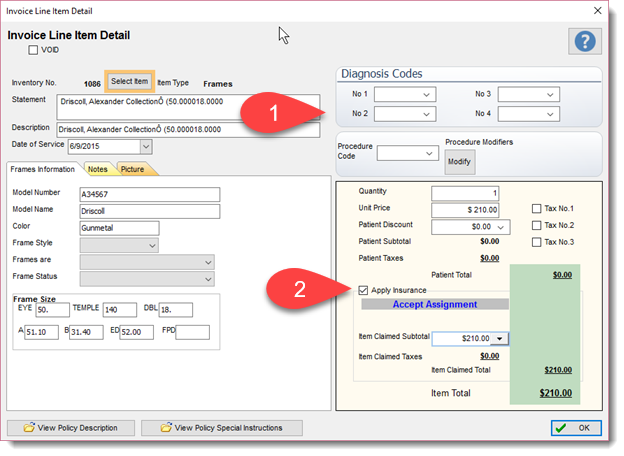
The actual claim billing values are entered in the Invoice Line Item Detail section for each item listed on the Invoice. In section 1, illustrated below, a user can enter the diagnostic codes, billing codes and any applicable modifier. Typically the billing and diagnostic codes are mandatory for claims to be validated and created.
IMPORTANT:
If you make a change to a value (price of an Item, CPT/ICD9/10 or Modifier once a claim has been prepared you must select the Prepare/Update button again for the claim to be updated. If you do not Prepare/Update the claim your changes will not be reflected in the Claim.
|
By placing a check mark in the Apply Insurance field (item 2) will cause Filopto to calculate the insurance claim to be generated using the rules defined by the user (in the Insurance Manager (billing rules) for the selected insurance company and policy) or by the manual entry done by the user of the values entered in this section.
The Check Mark also prepares the claim for recording in the Insurance AR. The claim will be recorded in the Insurance AR only once the claim has been created and submitted to the insurance processor. If a claim is never submitted the claim is never recorded as a receivable for accounting purposes.
The Insurance section ( lower left side of the invoice screen) display the Patient default insurance policies on record for the patient. If a Patient has multiple (default) policies registered, the section, will be automatically adjusted to display the polices such as shown below.
Note that the Claims button all show (0) for the number of claims created using the insurance policy shown.
The user can change the default insurance policies for a patient by selecting the drop down beside the appropriate insurance section.
Once a claim is prepared, the insurance policy for that selection cannot be changed. To change a policy once a claim has been created the claim must be first voided and then a new insurance policy can be selected.
Important:
Each policy has an effective date and expiry date. If these dates do not match the period for the claim the patient insurance policy will not be displayed in the drop down screen. If no insurance policy is selected you cannot create a claim.
Before generating an Insurance claim insure that you have properly completed the invoice and have included all necessary information and payments on the invoice before you generate the claim. Insurance claim that have been prepared and submitted to the insurance company can only be modified manually.
For the automated claim to function, the Insurance company must be selected prior to entering the invoice line item screen or selecting a line item to be billed.
|
To create a claim select the appropriate Claim button and a drop down screen containing the claim information will be displayed.
The Prepare / Update button will create or update an existing claim. Once a claim is prepared it will appear in the grid below the Prepare / Update button. You can view/edit the claim by double -clicking on the claim record in the grid.
WEB Base Claim submission
If you entered in the Insurance company profile a web site a Go To Insurance Website button is displayed permitting the user to enter, if appropriate, the claim via the insurance web interface or consult the insurance web site for information (see Insurance Companies and Plans). If you wish to track the account receivable of a web claim you will still need to create the claim in Filopto. However since you will not be generating an electronic claim you can place in the Insurance Company profile not to verify the claim information and Filopto will use the invoice information to create the insurance AR record.
|
If some patient information is missing a Message Dialogue box can appear (see claim verification) identifying the items that are missing to properly create a claim. Enter any missing information and then try again the Prepare/Update claim button and create the claim. The claim information looks in the Patient, Employee, System Settings and Insurance Company File for the information required. If you enter the data required in these files prior to creating the invoice no missing information warnings will appear.
Once a Claim is prepared at Invoice time, all claims are then batch for review and submission. To submit claims go to the Back Office - Patient and Insurance tab. Select the Send Claims to Insurance Companies button to view, review and send the claims that are ready. The action of sending the claims (or Printing the claims from the Send Claim to Insurance Companies) records the receivable into the insurance accounts receivable ledger.