
Background - USA
Evaluation and Management (EM) services refer to visits and consultations provided by physicians or residents under their supervision. Each of these services is assigned a CPT (Current Procedure Terminology) code for billing purposes. These codes were developed by the American Medical Association and implemented by HCFA in 1992, as part of the sweeping changed required by the resource-based Medicare fee schedule payment system. Like all CPT codes, EM codes are "universal" and used by Medicare, Medicaid and most other payor's for processing claims for the professional services of physicians. Since visit and consultation services are high volume physician activities, the EM codes are the most frequently used by physicians in daily practice.
How Physicians use EM Codes
To bill for a patient visit conducted at a clinic, office, hospital, emergency department or nursing home setting, a physician must select an EM code that best represents the service performed. EM codes are organized into various categories by delivery site of service, then into as many as five discrete "levels" or "established" patients. All these categories and code levels are intended to provide the physician with an opportunity to select the code that best reflects the extent of his/her personal work necessary to perform the visit service.
EM services are constructed on the basis of physician performance in three "key" elements of every visit or consultation service: patient history, examination and medical decision-making. Secondary factors for selecting a code include the activities of counseling, coordination of care, nature of the problem and the time spent "face to face" with the patient. As the degree of physician involvement and work intensity varies along the key components of history, exam and medical decision-making for any visit service performed, so does the level of code selected. The more work performed by the physician, the higher the level of code he/she may bill within the appropriate category.
Key Terms:
All physicians and qualified non-physician practitioners shall follow the E/M documentation guidelines for all E/M services. These rules are applicable for Medicare secondary payer claims as well as for claims in which Medicare is the primary payer.
New Patient: a patient who has not received any professional services from the doctor, or another doctor of the same specialty who belongs to the same group, within the past three years. Interpret the phrase “new patient” to mean a patient who has not received any professional services, i.e., E/M service or other face-to-face service (e.g., surgical procedure) from the physician or physician group practice (same physician specialty) within the previous 3 years. For example, if a professional component of a previous procedure is billed in a 3 year time period, e.g., a lab interpretation is billed and no E/M service or other face-to-face service with the patient is performed, then this patient remains a new patient for the initial visit. An interpretation of a diagnostic test, reading an x-ray or EKG etc., in the absence of an E/M service or other face-to-face service with the patient does not affect the designation of a new patient.
Established Patient: A patient who has received professional services within the past three years
Consult Patient: Type of service provided by doctors whose opinion/advice, regarding evaluation and/or management of a specific problem, is requested by another physician. Effective January 1, 2010, the consultation codes are no longer recognized for Medicare Part B payment. Physicians shall code patient evaluation and management visits with E/M codes that represent where the visit occurs and that identify the complexity of the visit performed.
Chief Complaint: A concise statement (usually in the patient's words) describing the symptoms, problem, condition, diagnosis, and or other factors that are the reason for the doctor/patient encounter.
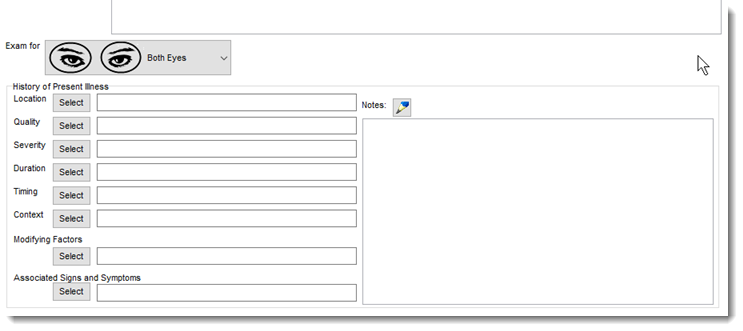
HPI: History of Present Illness. A chronological description of the development of a patient's present illness from the first sign/symptom to the present; includes a description of location,quality, severity, timing, context, modifying factors, and associated signs and symptoms significantly related to the present problem.
The E&M Code Verifier
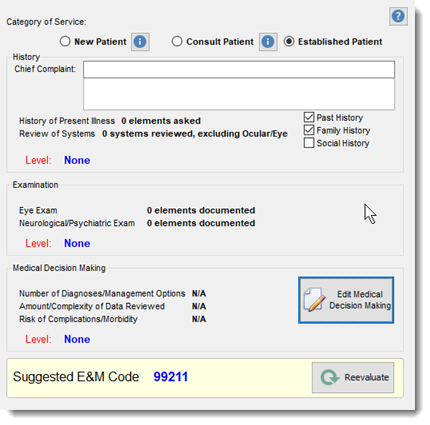
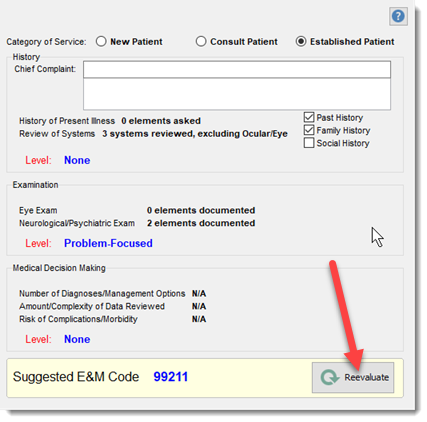
The E&M code verifier analyses the activities recorded by the provider in the EMR module and uses the HCFA E & M coding rules to evaluate and grade the effort required for the patient exam. The E&M code verifier evaluates the recorded information and categorizes the information in three areas:
1) Determine the amount of History obtained. To qualify for a given service level, all elements identified for that level must be met or exceeded the established HCFA standards.
2) Determines the extent of Examination performed. To qualify for a given service level, all elements identified for that level must be met or exceeded the established HCFA standards.
3) Determines the complexity of Medical Decision-Making involved. To qualify for a given service level, all elements identified for that level must be met or exceeded the established HCFA standards.
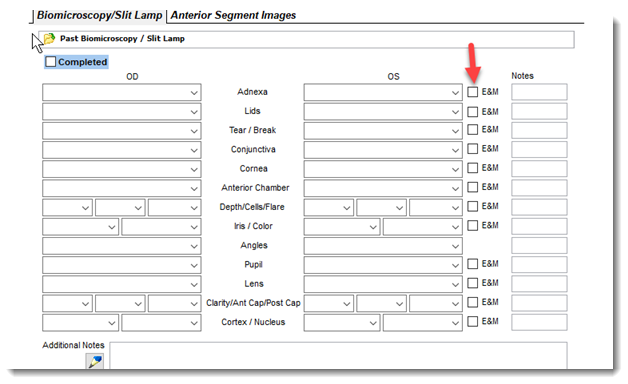
Several screens in Filopto have special fields that when check marked, will be used in the E/M Code verifier process. For example in the image below the fields identified as E&M are the fields used in the Code Verifier process. The provider should indicate by placing a check mark that he has completed this test per the E&M coding standard.
At billing time the provider can calculate and review the items completed used to calculate the suggested E&M code by selecting the Code Verifier option (2) in the billing (1) page. The provider can make any changes required to the exam record and recalculate the suggested E&M code.
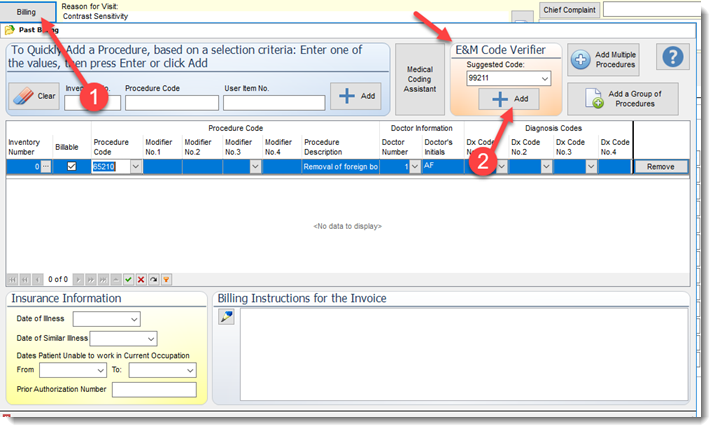
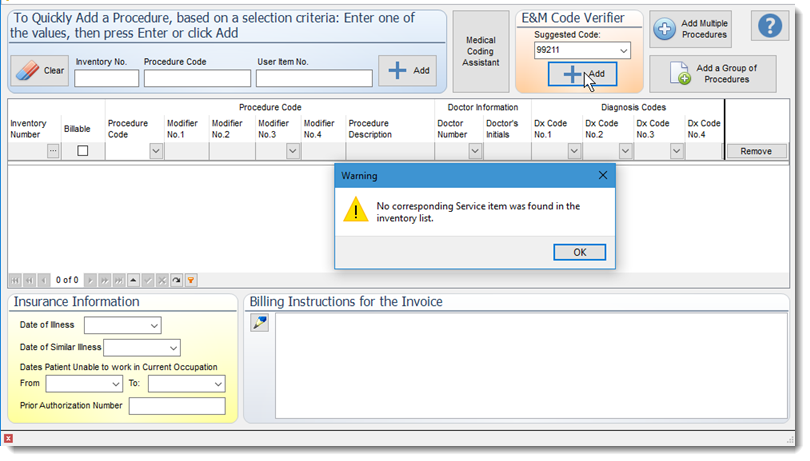
ADD E&M Code to Billing
To add the suggested E&M code to the billing screen select the add button in the billing page. If no inventory service item exist in your inventory item list for the selected E&M code you will receive a warning message to enter an inventory service item that has the matching CPT code into your Inventory service item list.
Reevaluate E&M Code
To reevaluate the suggested code (i.e. after making further changes to the exam records) select the Reevaluate button in the Evaluation & Management Code Verifier page.
References:
4. Medicare Learning Network Centers for Medicare & Medicaid Services http://www.cms.hhs.gov/MLNGenInfo
|
