The SOAP tab permits providers to record their findings based on the SOAP protocol. Each progress note is concern with a single problem and should be numbered and tittle accordingly. In an eye care practice, progress notes normally exist when the practitioner sees a patient on more than one occasion in relation to a particular problem(s).
Progress notes are of particular value to the eye care specialist when contact lens are fitted. Because contact lens tend to cause problems of their own, the careful recording of progress notes for each progress evaluation visit can give direction to the procedures performed at these visits and to the advise and instructions given to the patient. This also applies to patients undergoing vision therapy and low vision rehabilitation.
Each note is written in narrative form and should include four components:
Symptomatic
Objective
Assessment
Plan
This portion of the record system is known as the SOAP system. The progress notes are the final step in the feedback loop, often resulting in the formulation of additional plans that will be evaluated at additional progress visits. When a patient is being transferred from one particular practitioner to another, the final progress notes should emphasize the assessment of unresolved problems.
The four parts of a SOAP note are outlined below:

1. SUBJECTIVE/SYMPTOMATIC —The initial portion of the SOAP note format consists of subjective observations. These are symptoms the patient verbally expresses or as stated by a significant other. These subjective observations include the patient's descriptions of pain or discomfort, the presence of nausea or dizziness and a multitude of other descriptions of dysfunction, discomfort or illness the patient describes.
2. OBJECTIVE —The next part of the format is the objective observation. These objective observations include symptoms that can actually be measured, seen, heard, touched, feel, or smelled. Included in objective observations are vital signs such as temperature, pulse, respiration, skin color, swelling and the results of diagnostic tests.
3. ASSESSMENT —Assessment follows the objective observations. Assessment is the diagnosis of the patient's condition. In some cases the diagnosis may be clear, such as a contusion. However, an assessment may not be clear and could include several diagnosis possibilities.
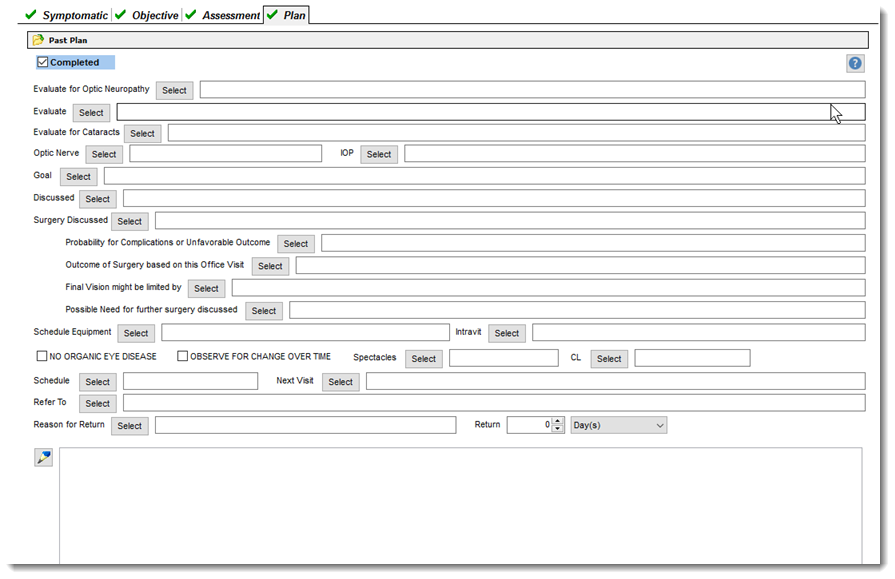
4. PLAN —The last part of the SOAP note is the plan. The plan may include laboratory and/or radiological tests ordered for the patient, medications ordered, treatments performed (e.g., minor surgery procedure), patient referrals (sending patient to a specialist), patient disposition (e.g., home care, bed rest, short-term, long-term disability, days excused from work, admission to hospital), patient directions and follow-up directions for the patient.
 The SOAP Note should briefly express the following:
The SOAP Note should briefly express the following:

(1) Date and purpose of the visit. The patient's symptoms and complaints

(2) The current physical exam. What is the patient's height, weight, temperature, pulse, blood pressure, visual acuity, etc.

(2) New lab data and results of studies, reports, assessments

(3) The current formulation and plan for the patient